Case Study: Lung Transplant Virtual Care Program

“We’ve had cases where the device detected problems before the patient noticed symptoms. Early detection allows a better chance at identifying a problem and applying the appropriate treatment plan."
- 427 patients enrolled remotely, 117 patients onboarded and enrolled in person
- 68% of patients engaged with chat
- 98% Patients submitted their symptom data
- $180,000 estimated total cost savings
(https://www.sciencedirect.com/science/article/pii/S105324982300030X?via%3Dihub)
Empowering Post-Lung Transplant Patients to Manage and Monitor Their Care
To prevent chronic rejection, lung transplant recipients are screened for lung function using pulmonary function testing (PFT) in a laboratory at regular intervals, frequently initially then semi-annually as time goes on.
While tests are important for patients to manage and monitor their wellbeing, the periods in between visits are just as crucial. Patients and providers needed a convenient way to bridge the communication during these “out-of-office” times so that any early indications of issues can be addressed immediately. An added inconvenience was that patients had to factor in time and travel for any in-person visits.
The solution came when the pandemic hit in 2020 – it put the health and safety of more than 500 lung transplant recipients at UCSF Health at risk. Pulmonary laboratories were forced to shut down because of the pandemic, and as patients were immunocompromised, their travel and exposure risk had to be limited.
What did we do?
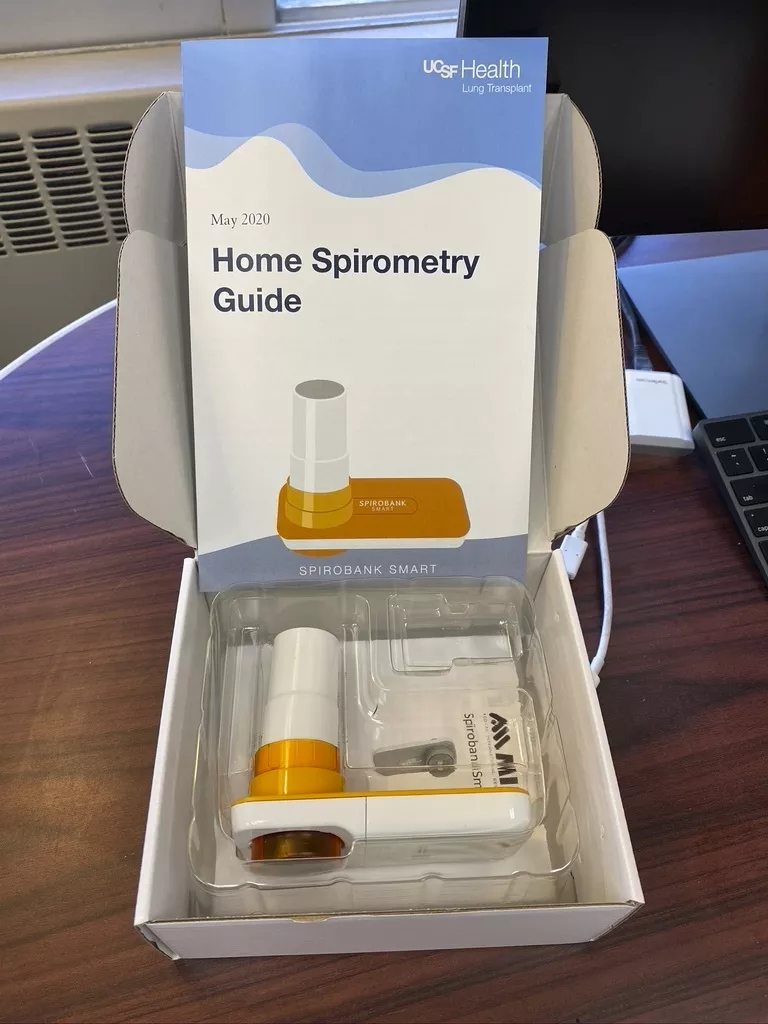
In May 2020, the UCSF Lung Transplant Program enrolled patients and mailed them Bluetooth- enabled home spirometry kits. It included instructions to enroll in a personalized digital health chatbot developed in collaboration between CDHI and Conversa Health.
While home spirometry devices were not new and already in use, it was difficult for patients to request and receive feedback, and physicians lacked the ability to actively monitor patient’s home measurements.
Patients were able to use their spirometers in their own homes and enter results into the chat. And an integration with Epic (Electronic Health Record) ensured that any concerning results were flagged and forwarded to the providers’ in-basket. Weekly patient summary reports were made available to providers to determine the next best action to take for the patient.
How it Works
1. Download the App
Patients download the app on their smartphone.
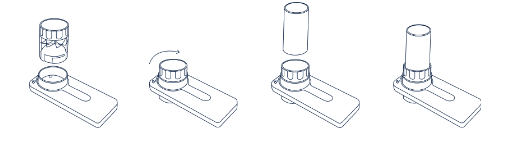
2. Assemble Device and Connect
Upon assembling the spirometer, the app will recognize the device.
3. Take Measurements
Patients take their first measurement by taking in a full breath in and then forcefully blowing it out for at least six seconds and until all the air is out of their lungs. The test should be taken three times. In the results, FEV1(L) records the amount of air the patient can force from their lungs in one second.
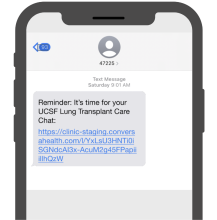
4. Text or Email Reminders
Patients will receive a text (SMS) or email reminder with a link when it is time to use the spirometer. Patients can also enter their FEV1 value as often as needed.
5. Lung Transplant Care Chat
Patients can engage in automated chats about their lung health. When it’s time for a chat, they will receive a reminder with a link where they will enter their FEV1 value and answer lung health questions. The UCSF Lung Transplant care team will access the answers after the chat and if the patient’s FEV1 is far below the baseline, they will be notified and contact for additional questions.
6. Communicating with the Nurse Coordinator
Patients can contact their nurse coordinator if there is a 10% change in their FEV1 for three days in a row or if they have any symptoms like shortness of breath (even if their FEV1 is stable).
What Was Our Impact?
The a clinical check-in gap between patient and provider is decreased as patients can now
have the ease and convenience of connecting via the chatbot and home spirometry kit, and
providers can know more—and worry less—about their patients’ health between visits or
emergencies.
Since its launch,
- About 544 post-lung transplants patients are enrolled,
- 68% have engaged with the chat, and
- 6 in person visits per patient have been replaced by home testing and video visits during first two years after lung transplant
Usage statistics show high engagement, and most importantly, the practice can quickly find out
if there is a problem, giving doctors the ability to intervene early and ensuring immediate action
in the event of severe symptoms of rejection.
Testimonials
Patient: Brad dell video? https://vimeo.com/478700569
Patient quotes: “You are all amazing
“It keeps you connected with the clinicians.”
“...having the assurance of the device is really helpful for me to know that I can test my lung function whenever, wherever.” – Brad, UCSF post lung-transplant patient
For more information on the lung transplant virtual care program